Local nurse practitioner appreciates the little joys during first year at UMMC

Perspective is everything, so the saying goes.
And for one nurse practitioner at Batavia’s United Memorial Medical Center, it’s been a lesson worth remembering from this past year of all things COVID-19.
“I didn’t expect to lose so many people in a year. The wins are great; it’s so awesome to take a breathing tube out and hear them saying good morning to you,” Marie Campbell said during an interview with The Batavian.
“I was hoping for more wins than losses … it’s one hour, one day, one minute at a time.”

Campbell, originally from Connecticut and a current resident of Akron, first joined the Air Force on her way to a medical career path. It was while stationed In Texas that she met her future husband Bill. They moved to his hometown of Akron and had three boys, James, now 7, Alexander, 4, and 18-month-old Malcolm. Mrs. Campbell wanted to find a job that was “exciting and interesting,” she said, and opted to attend D’Youville College and University at Buffalo, eventually completing her Doctor of Nursing Practice.
Once done with the educational portion of learning, Mrs. Campbell landed a job in the neurological Intensive Care Unit at Buffalo General, and then in the ICU at UMMC a year ago Nov. 30. To bump up the stress another notch, she was pregnant during those first tenuous months of the pandemic, giving birth to Malcolm in May 2020.
Mrs. Campbell was shielded from COVID-19 patients initially, she said, until after she gave birth. When she first came onto the ICU floor, it was a safety protocol all the way, she said: Here’s your N95 mask, gloves, gown, and special headgear.
“It’s scary,” Mrs. Campbell said. “I’m changing my clothes in the garage and I don’t go into the house … it’s really tough when three kids want to tell me about their day.”

As a nurse practitioner, she deals a lot with the families of patients, explaining what’s going on and what the medical treatment plan entails. Patients with COVID-19 could not have visitors whereas those with illnesses other than the virus could.
“Most of the interactions with families were on the phone,” she said. “COVID patients don’t get visitors unless they’re end of life. I’ve lost track of all the patients we’ve lost over the last year; I’ve stopped counting.”
One of the most difficult talks she has with patients is that they need a breathing tube and be intubated. “That terrifies people,” she said, “and family members are terrified.”
“In people’s mind, if you put a person on a breathing tube, they won’t survive,” she said.
Although that’s not true, it’s what many people have come to believe about having that tube down their throat, she said. Those with COVID-19 are more often than not unvaccinated and in their 50s and 60s, she said. Their reasons for not getting the shot vary, from their belief it is not safe and decisions to wait awhile longer to see more results, to not thinking the virus is a real threat, she said.
“Being vaccinated makes a difference; it does not mean you’re 100 percent safe, but it does make a huge difference in going into the ICU,” she said. “A large percentage of those not vaccinated … end up getting really sick.”
Her job also includes performing intubations, putting in central lines (which are larger IVs), and reviewing patient charts and lab results. The challenges of a pandemic and constant loss of life have been outweighed by the less intrusive rewards.
“As hard as it was, it was the right decision for me,” she said, highlighting a perk of her job. “The feeling I can make a difference in someone’s life. Often they’re very, very sick, and I can talk to their families. Being able to talk to them, explain things to them … giving them comfort in knowing we’re doing everything we can.”

Despite their tender ages, her children seem to be quite aware of COVID-19 and what it means. She laughed when describing a time she was carrying her 18-month-old son into a medical office, and he reached over to grab some hand sanitizer.
There are also those sad times, she said. The 35-year-old has been surprised, given she’s in a “small community hospital,” to see the number of sick people coming through the door. Her husband contracted COVID-19 before the vaccine was available to him, and he has since gotten it. The couple is thankful he did not suffer the serious side effects known to so many. Those others have not been as fortunate, she said.
“There are multiple people who wished they had gotten vaccinated, and they passed away,” she said, sharing a piece of advice she’s had to embrace. “When you leave work, you just have to leave it at work. My focus is being at home, enjoying my family.”
One such patient — a gentleman who had gotten the virus at a wedding — came to her mind. His last words were that “I never should’ve gone to that f- - - ing wedding.” He then died.
It hasn’t all been so bleak, though, Mrs. Campbell said. Many younger patients have gone on to do “really well” and get discharged, even after being on a ventilator.
“It does happen; the tube is removed and they go home,” she said. “And those are always the best ones.”

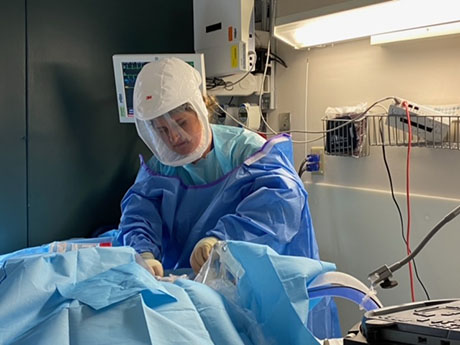
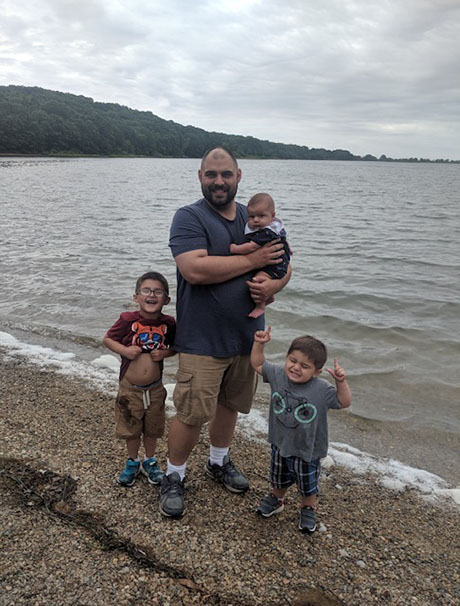
Top photo: Marie Campbell, a nurse practitioner at UMMC in Batavia, enjoys time spent with her family, including son Malcolm, 18 months. Sons James, 7, and 4-year-old Alexander also look forward to being with mom, who works with a patient on the Intensive Care Unit floor at UMMC, and dad, Marie's husband Bill, above.














